COVID-19 Immunity May Last Six Months or More
HHMI-- Press Release: Nov 11, 2020 Howard Hughes Medical Institute People who have recovered from coronavirus can make
potent antibodies to SARS-CoV-2 that evolve in the months after infection. These antibodies may be evolving in response to residual viral antigen hidden in the gut.
HHMI scientists are joining many of their colleagues worldwide in working to combat the new coronavirus. They’re developing diagnostic testing, understanding the virus’s basic biology, modeling the epidemiology, and developing potential therapies or vaccines. We will be sharing stories of some of this work.
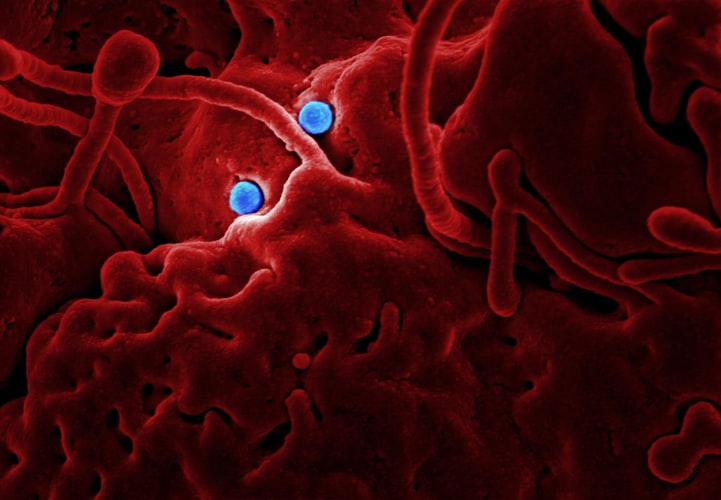
Scientists found traces of SARS-CoV-2 (green) in cells lining people’s intestines three months after infection. Antibodies may evolve in response to these residual viral traces. Credit: C. Gaebler et al./bioRxiv.org 2020
Around the world, coronavirus cases are surging and deaths due to the disease keep ticking up – more than 240,000 in the United States so far – but a new antibody analysis offers a hint of hope.
People who doctors consider to be recovered from the disease produce virus-fighting antibodies that rapidly evolve in the months following an infection, Howard Hughes Medical Institute Investigator Michel Nussenzweig’s team reports. Six months after infection, those antibodies become both more potent and better at combating mutated versions of the virus, called SARS-CoV-2.
The work, posted as a preprint to bioRxiv.org on November 5, 2020, has not yet undergone the scientific vetting process known as peer review. But the results suggest that the immune systems of previously infected people might have defenses ready if exposed to the virus again, says Nussenzweig, an immunologist at The Rockefeller University, in New York City. “The really good news is that people who are infected are very unlikely to become sick again for at least six months.”
The study is critical for scientists trying to understand just how durable people’s immune responses really are, says Leo Stamatatos, an immunologist at the Fred Hutchinson Cancer Research Center, who was not involved with the work. “This work suggests that our bodies can remember SARS-CoV-2 for at least half a year – and probably longer,” he says. “That’s a good thing.”
The long haul
Nussenzweig’s team first began recruiting people who had recovered from coronavirus disease, called COVID-19, in April, during the height of the pandemic in New York. At the time, the state’s case count was approaching 10,000 per day, and hospitals faced a deluge of sick people being treated in intensive care units and on ventilators.
The researchers collected blood from 149 participants and combed it for immune cells that make protective antibodies – those that zero in on the virus and block its entry into cells. “Our idea was that if we’re able to find such neutralizing antibodies, we would know what part of the virus vaccines have to target,” Nussenzweig says. These antibodies might also serve as a blueprint for a new drug – molecules that scientists could purify, produce in mass quantities, and then give to patients to prevent or treat COVID-19.
Nussenzweig and his colleagues reported their first big find in the journal Nature, in June. One month after infection, all 149 participants had coronavirus-fighting antibodies. “Our results showed that it’s not hard for our immune systems to make effective antibodies to SARS-CoV-2,” says Christian Gaebler, a physician and immunologist in Nussenzweig’s lab.
The level of these antibodies in the blood was generally low, but their presence in so many people was a bright sign for vaccine development. A vaccine that boosts production of these antibodies could be effective in a broad population of people, the team suggested.
Nussenzweig’s team took a closer look at the antibodies of six participants and discovered antibodies that were especially effective. Over the last few months, his lab has worked on more than a dozen studies examining two of these exceptional antibodies. Combined in a cocktail, they can protect mice from SARS-CoV-2 infection, the researchers reported in September, in a study later published in the Journal of Experimental Medicine. The team has also seen promising results in rhesus macaques. “These antibodies are very, very potent,” Nussenzweig says. His team is planning a Phase 1 clinical trial to test the safety of the antibodies in people. But a potential therapy could still be a long way off.
In the meantime, “One of the things people worry about a lot is what’s going to happen in six months or a year,” Nussenzweig says. “Are individuals who’ve recovered from COVID-19 still going to be protected?”
Staining for SARS-CoV-2’s shell (green) in samples of intestinal biopsies revealed that the virus (or pieces of it) may be hiding out in people’s gut. Scientists do not yet know whether these viral stowaways are infectious or produce clinical symptoms. Credit: C. Gaebler et al./bioRxiv.org 2020
A link to the gut
At the end of August, Nussenzweig’s team began bringing back their study participants for a second round of investigation. Over a period of six weeks, the researchers collected blood from 87 of the original 149 volunteers. “We just wanted to take a look and see if the antibodies were still there,” Gaebler says.
And they were, the team discovered, though levels had dropped – by more than 50 percent, in some cases. But that’s normal for infections, he says. More promising was the participants’ memory B cell levels, which stayed steady. These immune cells remember pathogens they’ve seen and crank out new antibodies when those pathogens come around again.
Each memory B cell contains genetic instructions for making antibodies. When the team examined these cells in the six participants from their earlier study, they found something remarkable. In the roughly five months since the original study, these participants’ memory B cells had picked up genetic mutations that altered the antibodies they produced.
Signs of the novel coronavirus are visible in these electron microscopy images of tissue from the gut. At right, red dots indicate surface spikes on viral particles. Left scale bar equals 0.2 micrometers; right scale bar equals 0.1 micrometers. Credit: C. Gaebler et al./bioRxiv.org 2020
Some mutations led to antibodies that were better at latching on to SARS-CoV-2, or to variants of it created in the lab. “Everything about this surprised me,” Nussenzweig says. “I didn’t expect that we would find these mutations.”
Antibodies often evolve like this when there’s a chronic infection, such as with HIV or herpes, where virus lingers in a person’s tissue and cells. But coronaviruses typically clear out from the body quickly after infection, Gaebler says, so he wouldn’t have expected the immune system to keep refining SARS-CoV-2 antibodies.
Maybe residual viral particles are hiding out somewhere, the team surmised. They decided to go fishing in the gut. (Like the lungs, people’s intestines are carpeted with the kind of cells SARS-CoV-2 can invade, Nussenzweig explains.) They teamed up with physicians from Mount Sinai Hospital and examined biopsies from seven of 14 patients who had recovered from COVID-19. In the intestinal tissue, the researchers found viral traces, including SARS-CoV-2’s telltale crown of spikes. “The images are quite striking,” Gaebler says.
It’s possible that antibodies mutate in response to the residual viral antigen tucked away in people’s bowels, Nussenzweig says, though there may be other caches of coronavirus in the body.
What’s still remains to be discovered, he says, is whether these viral stowaways have any clinical relevance – if people who carry virus in the gut, for instance, are more likely to be “long-haulers” with lingering symptoms, or if these virus particles are even infectious.
###
Citations
Christian Gaebler et al. “Evolution of Antibody Immunity to SARS-CoV-2.” Posted on bioRxiv.org on November 5, 2020. doi: 10.1101/2020.11.03.367391
*Alexandra Schäfer et al. “Antibody potency, effector function and combinations in protection from SARS-CoV-2 infection in vivo.” Posted on bioRxiv.org on September 15, 2020.
Davide F. Robbiani et al. “Convergent antibody responses to SARS-CoV-2 in convalescent individuals.” Nature. June 18, 2020. doi: 10.1038/s41586-020-2456-9
*Editor’s note: The Schäfer et al. study was published in the Journal of Experimental Medicine on November 19, 2020.
Scientist Profiles
https://www.hhmi.org/news/covid-19-immunity-may-last-six-months-or-more
Michel C. NussenzweigThe Rockefeller UniversityImmunology
Molecular Biology
FOR MORE INFORMATION
Meghan Rosen301-215-8859rosenm2@hhmi.org


 How to resolve AdBlock issue?
How to resolve AdBlock issue? 